Why Do East Asians Bleed More on Heart Medications? New Guidelines Change Everything
The East Asian Paradox Finally Gets Official Recognition
Have you ever wondered why your grandmother's heart medication dosage differs from what Western guidelines recommend? A major breakthrough published in JACC: Asia this July 2025 might finally explain why. Leading cardiologists from South Korea, China, Taiwan, and Singapore have released comprehensive antiplatelet treatment guidelines specifically designed for East Asian patients, marking a historic shift in cardiovascular medicine.
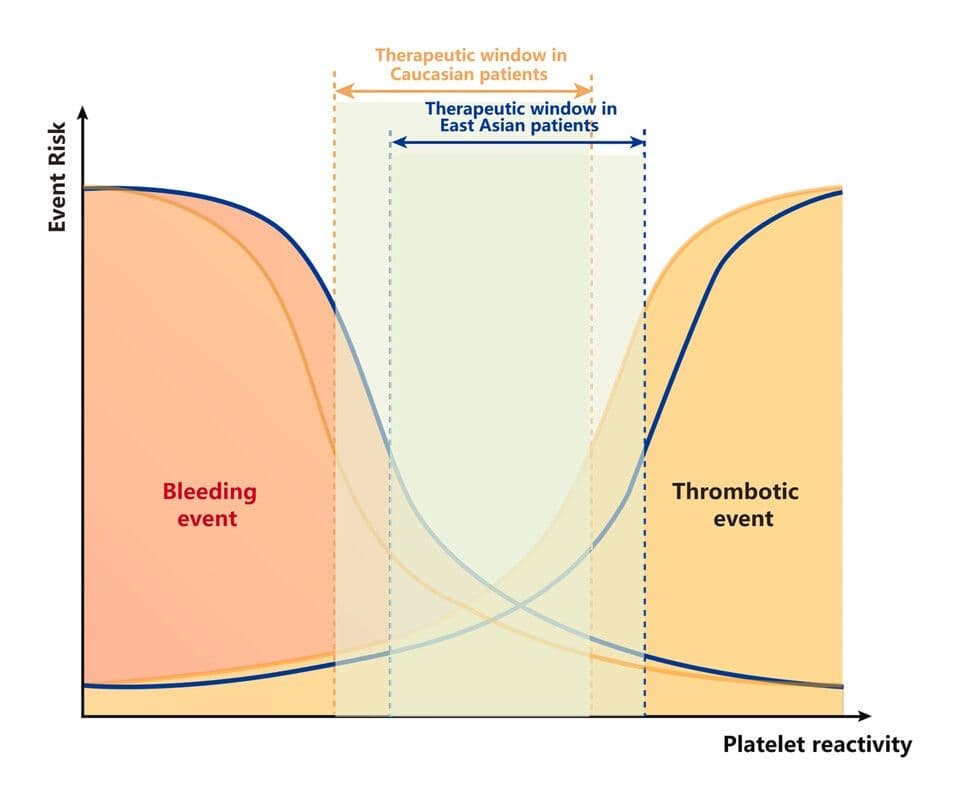
At the center of this medical revolution stands Professor Jung Young-hoon from Chung-Ang University Gwangmyeong Hospital, who first proposed the East Asian Paradox concept back in 2012. This paradox describes a puzzling phenomenon: East Asian patients show lower responsiveness to clopidogrel, suggesting higher blood clot risks after stent procedures. Yet paradoxically, they experience fewer thrombotic events and significantly more bleeding complications compared to Western patients. After more than a decade of research, this observation has evolved from a curious anomaly into a cornerstone of treatment strategy design.
The new guidelines represent a collaborative effort involving top cardiovascular experts across East Asia, providing concrete evidence that one-size-fits-all Western protocols may be doing more harm than good for approximately 25% of the global population living in this region.
Why Western Standard Doses Lead to Dangerous Bleeding

The consensus document highlights a critical safety concern: P2Y12 inhibitors like ticagrelor and prasugrel, considered gold-standard treatments for acute myocardial infarction in Europe and America, carry substantially higher bleeding risks when used at full Western doses in East Asian patients without providing additional ischemic protection.
Large-scale clinical trials conducted in South Korea and Japan revealed striking results. Ticagrelor increased bleeding rates by up to twice compared to clopidogrel, yet showed similar effectiveness in preventing ischemic events. This finding challenges the assumption that more potent antiplatelet therapy automatically translates to better outcomes for East Asian populations.
Consequently, the guidelines strongly recommend limiting high-intensity antiplatelet treatment with standard-dose ticagrelor and prasugrel to just 1-3 months in most cases. After this initial period, physicians should consider aspirin discontinuation, dose reduction, or switching to clopidogrel through stepwise de-escalation strategies. Professor Jung emphasized that Western bleeding risk assessment tools like ARC-HBR fail to adequately account for the physiological and physical characteristics of East Asian patients, including lower body weight thresholds for men under 55kg and women under 50kg, as well as frailty factors that demand more sophisticated evaluation criteria.
Clopidogrel Over Aspirin for Long-Term Protection
Beyond emphasizing early dual antiplatelet therapy de-escalation, the guidelines introduce another paradigm shift by advocating for early conversion to monotherapy with a preference for clopidogrel over the traditionally favored aspirin for long-term maintenance.
Several pivotal clinical trials conducted across East Asia, including HOST-EXAM, SMART-CHOICE 3, STOPDAPT-2, and STOPDAPT-3, consistently demonstrated that long-term clopidogrel monotherapy did not increase bleeding risks compared to aspirin monotherapy, while significantly reducing ischemic event occurrence. The HOST-EXAM study, which followed 5,530 patients who received drug-eluting stents, showed that clopidogrel outperformed aspirin in preventing death, stroke, and bleeding complications over extended follow-up periods.
These findings reflect clinical reality: prolonged dual antiplatelet therapy in East Asian patients fails to reduce ischemic events while substantially elevating bleeding risks. Medical communities and patients across Korea, Japan, and China have actively discussed these research outcomes on platforms ranging from Naver blogs to medical forums, with many expressing relief that treatments are finally being tailored to Asian physiology rather than simply adopting Western protocols.
A New Treatment Paradigm for 1.6 Billion People
Professor Jung Young-hoon, who also serves as hospital director and leads the Thrombosis and Biomarker Center at Chung-Ang University Gwangmyeong Hospital, describes this consensus document as the starting point for a new treatment paradigm applicable across the entire East Asian region. His vision extends beyond current guidelines to developing comprehensive risk assessment systems and standardizing treatment protocols through continued research collaboration with the Chinese Society of Cardiology and other regional partners.
The East Asian Paradox is no longer merely an initial observation but has become a core concept in treatment strategy design, Jung emphasized. He expressed hope that this consensus will serve as the foundation for establishing Korea-specific antiplatelet therapy strategies that could eventually influence global cardiovascular medicine. Recent research from his team has also identified coagulation intensity as a critical prognostic factor in high-risk patients, suggesting that future cardiovascular treatment might shift dramatically beyond the current dual antiplatelet therapy paradigm.
For international readers and expats living in East Asia, this development carries practical significance: if you or family members undergo cardiac procedures in this region, expect treatment protocols that may differ substantially from Western standards—not due to inferior care, but because of cutting-edge precision medicine recognizing fundamental biological differences between populations. The medical world is finally acknowledging that what works in Berlin or Boston may need careful adjustment for patients in Beijing or Busan.
Discover More
South Korea's October Heat Wave Hits 37°C: Why Is It So Hot in Fall?
South Korea experiences unprecedented October temperatures reaching 37°C with heat wave warnings across the nation. The extreme weather continues a pattern of record-breaking heat throughout 2025, raising concerns about climate change impacts.

When Flames Met Fate: The Seosan Restaurant Fire That Had Everyone Talking
A restaurant fire in Seosan's Daesan-eup on July 24, 2025, resulted in 150 million won in damages but fortunately no casualties. The blaze, which took two hours to extinguish, highlights growing concerns about fire safety in South Korea's industrial regions.